Happy Fall! We hope this Newsletter finds you well and we hope you enjoy!
19th Anniversary Gala – Update
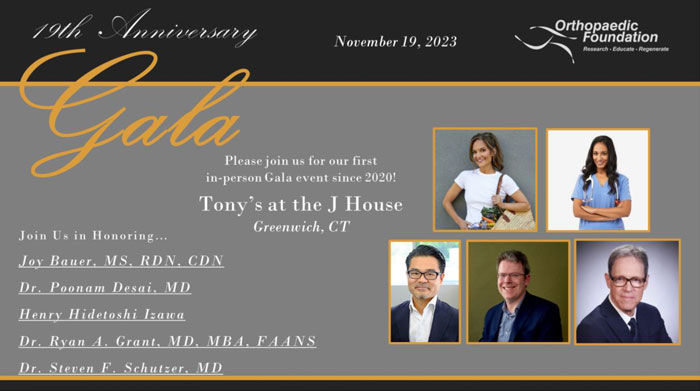
We are thrilled to announce the addition of our fourth and fifth Honoree to this year’s Gala event! We extend a warm welcome to Dr. Steve F. Schutzer, MD and Henry Hidetoshi Izawa to our list of Honorees for this year’s 19th Anniversary Gala.
Dr. Schutzer is a practicing orthopaedic surgeon specializing in hip and knee surgery, Co-Founder of Upswing Health, Physician Executive for Trinity Health of New England, and Co-Founder and Board
Member of the Connecticut Moving To Value Alliance. He is a Founding Member of and served as the Medical Director for the Connecticut Joint Replacement Institute from 2007-2021.
Henry Hidetoshi Izawa is President and CEO at Fujifilm Healthcare Americas. He is expertly skilled in medical devices, product marketing, and new business development. We look forward to honoring both Dr. Schutzer and Mr. Izawa at this year’s Gala on November 19th!
Fellows’ Graduation and West Point Sports Medicine Conference

On June 23rd, the Foundation’s two Sports Medicine Fellows presented their research at the annual Fellows’ Sports Medicine Conference at West Point! Dr. Alexander Strassman presented his research, entitled “Transtibial Anterior Cruciate Ligament Reconstruction using Age-Matched Patellar Tendon Autograft or Allograft”. Dr. Rafael Sanchez presented his research, entitled “Resorbable Bovine Patch Augmentation in Arthroscopic Rotator Cuff Repair: Impact on Clinical Outcomes in Patients with Medical Comorbidities.” Great job, Fellows!
Congratulations Drs. Sanchez and Strassman for fellows on completing their fellowship! The fellows formally graduated from the Fellowship program on July 25th. They will be returning to Miami, Florida and southern Wisconsin, respectively, to practice.
Manhattan Medical Immersion Camp

Our second annual Manhattan Medical Immersion Camp was a huge success! The students learned and practiced hands-on skills in a wide variety of medical specialties, including orthopaedics, dermatology, regenerative medicine, anesthesiology, nursing, vascular surgery, and more. We thank the staff, faculty, parents, and students for helping us make this year’s program better than we ever expected.
Please visit our website to sign up for more information and to be the first to apply to next year’s session. Be sure to check out and follow our Instagram feed at @ortho_foundation for exciting coverage of this year’s camp!
Research Corner
The Orthopaedic Foundation engages in research to discover new modalities for the treatment of orthopaedic injuries and musculoskeletal disease, to promote injury prevention, and to explore minimally invasive treatments that guarantee shorter recovery time and faster return to daily activities to help you lead a healthy and active lifestyle. A main focus our research is to provide alternative solutions to total knee replacement (TKR) for patients suffering from debilitating knee pain associated with knee arthritis.
Our research team published an article in the July 2023 issue of the American Journal of Sports Medicine entitled, Return to Sport in Middle-aged and Older Athletes After Unicompartmental Knee
Arthroplasty at a Mean 10-Year Follow-up: Radiographic and Clinical Outcomes. One-hundred sixty- nine athletes underwent unicompartmental knee arthroplasty (UKA) for either medial (inside) or lateral (outside) compartment knee osteoarthritis (OA). Ninety-eight percent of patients returned to vigorous and moderate sports at an average of 5-6 months after UKA. Of those that returned to sport, 99% were still participating in their sport of choice at an average of 10 years from their surgery. Sports included tennis, downhill skiing, and golf. These data demonstrate that UKA is a successful alternative to TKR in patients with single compartment knee OA in the appropriately- selected patient and allows patients to return to a healthy and active lifestyle. If you have isolated knee OA-related pain, you might be an eligible candidate and should consult a physician to discuss potential alternatives to TKR.
If you know someone that is suffering from mild to moderate knee osteoarthritis, contact our research team here to learn more about our clinical trial opportunities to help you stay in the game for life!
Interested in participating in clinical trials?
If you or someone you know someone that is suffering from a knee cartilage defect or mild to moderate knee osteoarthritis, contact our research team here to learn more about our clinical trial opportunities to help you stay in the game for life!
Roundtable Discussion
Q: How do you safely return to sport after a shoulder dislocation?
A: Overall, the treatment of shoulder instability largely depends on the type of instability the patient is experiencing. Like any other injury, the management of shoulder instability should begin with a thorough physical examination and detailed history. It is imperative to determine the patient’s goals and understand what activities they are hoping to return to, as this can have a significant impact on their rehab and timing for return to sport. In general, the management of a first-time shoulder dislocation remains challenging and is truly determined by the patient’s demands, risk factors, and expectations. Care typically begins with immobilization in a sling and is followed by early motion. If the patient is in-season and nonoperative management is decided upon, bracing during sports canbe utilized. Return to play is generally tolerated within the timeframe of 2-4 weeks and is after the patient is able to perform sport-specific activities without pain and their strength and range of motion have returned to pre-injury. Regardless, it is essential to counsel patients about the risk of future dislocations, especially in younger, more high-demand patients.
Many thanks to our very own Shoulder & Elbow fellow, Dr. Christopher M. Spolarich, MD, for this newsletter’s Roundtable Discussion! Dr. Spolarich completed his orthopaedic surgery residency at Summa Health System in Akron, Ohio. He is currently completing the Shoulder and Elbow Fellowship (ASES) at Plancher Orthopaedics & Sports Medicine.
Six Steps to Stronger Bones

Here are six great lifestyle tips that you can incorporate into your daily life to help strengthen your bones! Many thanks to Good Housekeeping for its contributions to the below segment.
- Limit salt and sugar intake – Ingesting excessive amounts of salt or salty foods depletes your body’s calcium stores. High amounts of sugar interfere with new bone formation.
- Correct your posture – Sitting hunched over puts unnecessary pressure on your spine. Since bones constantly break down and build up, sitting hunched over can cause those bones to reform in an awkward way, causing discomfort.
- Watch what you drink – Make sure to drink coffee and carbonated drinks in moderation, as recent research shows a link between these drinks and weaker bone structure.
- Limit alcohol intake – Too much alcohol throws off the body’s calcium balance. Experts recommend sticking to one serving per day at the most.
- Quit smoking – Studies show that tobacco users have lower bone mineral density on average, meaning their bones are less firm. This is because nicotine slows the production of bone-forming cells.
- Consider medication alternatives – Some medications have a demineralizing effect on your bones. If you have weak bones and also take steroids, proton pump inhibitors, aromatase inhibitors, some seizure medications, blood thinners, or diuretics, it may be worth it to seek alternatives with your doctor. The health benefits of these drugs may outweigh the risks, but it may be worth it to discuss with your doctor.
Spinach & Mushroom Quiche
This easy, delicious, and bone-healthy recipe is a crowd-pleaser for any brunch gathering. This recipe is vegetarian, gluten-free, and full of nutrients and vitamins from the eggs, spinach, mushrooms, and onions inside. The eggs are a fantastic source of protein and a variety of vitamins, while the spinach and onions are a great source of calcium. This quiche is crust-free too, getting rid of much of the hassle and making this recipe simple. Many thanks to Jessica Ball, MS, RD,
and EatingWell for its contributions to this recipe.
Ingredients:
- 2 tablespoons of extra-virgin olive oil
- 8 ounces of sliced fresh wild mushrooms (for example, cremini, button, oyster, or shiitake)
- 1-1/2 cup of thinly sliced sweet onion (or yellow onion)
- 5 ounces of chopped fresh baby spinach (about 8 cups)
- 6 large eggs
- 1/4 cup of whole milk
- 1/4 cup of half-and-half
- 1 tablespoon of fresh thyme leaves
- 1-1/2 cup of shredded Gruyère cheese
- Salt and pepper
Directions:
- Preheat oven to 375 degrees. Grease a 9-inch pie pan with cooking spray.
- Heat the olive oil in a large skillet over medium-high heat. Add the mushrooms and cook until tender
and browned (about 8 minutes). Add the onion and garlic and sauté until softened (about 5 minutes). - In a medium bowl, whisk the eggs, milk, half-and-half, thyme, mustard, salt and pepper in a medium bowl. Fold the mushroom mixture into the egg mixture, then fold in the shredded cheese. Spoon the
mixture into the greased pie pan. - Bake the quiche until set and golden-brown (about 30 minutes). Let it sit for 10 minutes to cool down.
- Enjoy!
This easy, nutritious, crowd-pleaser is full of vitamins and minerals and is a great way to feed a group of people and still eat healthy!
We hope you enjoyed this Newsletter, and we thank you for your continued generous support!
Warm regards,
Janine Bahar
Executive Director

Orthopaedic Foundation
Ph: 203-869-2002
www.ofals.org
